Bioinformatics & Genomics
Biophysics & Structural Biology
Biotechnology
Cancer Biology
Cancer Immunology and Immunotherapy
Cardiovascular Disease
Cell Biology
The Biomedical Sciences Graduate Program (BIMS) at UVA is a vibrant interdisciplinary graduate program committed to training PhD candidates in becoming the next generation of scientific leaders. We achieve this goal through an immersive curriculum coupled with rigorous research training and by providing students with the flexibility to tailor independent programs of didactic coursework. In parallel, we offer students a broad spectrum of research opportunities, delivered in partnership with the School of Medicine, Graduate School of Arts and Sciences, and School of Engineering and Applied Sciences at the University of Virginia.
Read about the many distinguishing features of our program and how you can train under world-renowned scientists who are committed not only to scientific discovery but also to mentoring and teaching.
Our distinguished faculty and cutting-edge curriculum empower future leaders in biomedical research to tackle today's complex challenges with passion and expertise.
Our deadline for Fall 2024 admission was December 1, 2023, and applications are currently under review. The application portal will open on September 1, 2024, for Fall 2025 admission.
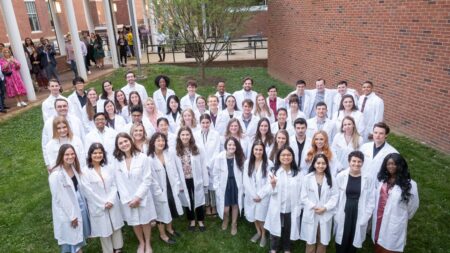
Biomedical Sciences Graduate Program 2023 Lab Coat Ceremony
The School of Medicine celebrated the UVA Biomedical Sciences Graduate Program (BIMS) Lab Coat Ceremony on April 14. This event marks the transition of our first-year BIMS students to the next phase of their graduate careers as they embark upon their mentored research projects. A total of 55 students were recognized in the following disciplines: Biochemistry and Molecular Genetics (9), Biomedical Engineering (2), Biophysics and Physiology (4), Cell Biology (7), Experimental Pathology (4), Microbiology (14), and Neuroscience (13). The class is 64% female and 22% of the total students are from underrepresented minorities (URM).
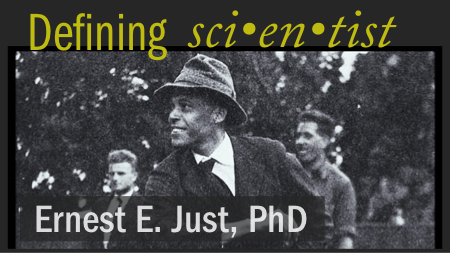
Researchers who changed how we view science
Ernest Everett Just, PhD (1883 - 1941), graduated Magna Cum Laude from Dartmouth College in 1907 with four bachelor's degrees, and received his PhD from University of Chicago in 1916. Author of more than 70 scientific papers and the text, The Biology of the Cell Surface (1939), we are spotlighting Dr. Just as our inaugural minority researcher in our series "Defining sci-en-tist".